Why Choose Tibial Interlocking Nail for Fracture Treatment?
In recent years, the use of Tibial Interlocking Nails has become increasingly popular for treating fractures. Dr. James Smith, a leading orthopedic surgeon, states, "The Tibial Interlocking Nail offers superior stability and promotes faster healing." This innovative device allows for precise alignment of the bones. It enhances patient recovery and improves outcomes.
Fractures can be complex injuries requiring careful intervention. The Tibial Interlocking Nail provides a stable fixation mechanism. This technique addresses various fracture types, including complex and comminuted scenarios. Surgeons find it advantageous due to its versatility and effectiveness.
However, not every patient experiences the same results. Some may face complications, such as infection or improper alignment. Continuous evaluation and adaptation of surgical techniques are crucial. The Tibial Interlocking Nail is not a one-size-fits-all solution. It prompts discussions among healthcare providers about best practices for each unique case. Balancing innovation with patient-specific needs remains a challenge in orthopedic care.
Overview of Tibial Interlocking Nail Technology
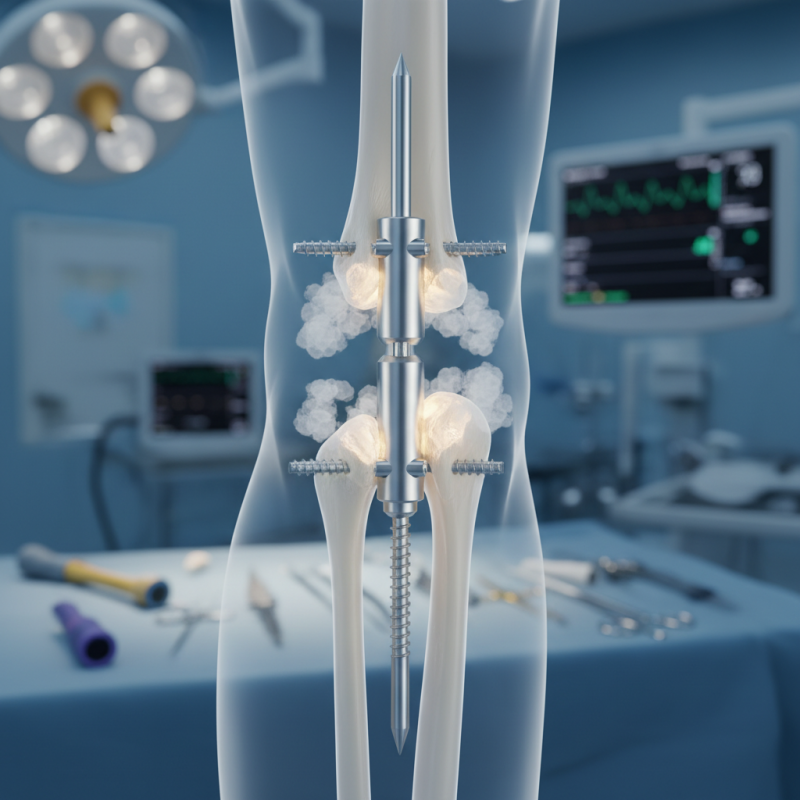
Tibial interlocking nail technology has gained popularity for treating fractures. This approach offers advantages over traditional methods. It stabilizes the broken bone and aids in healing. The design of the nail allows for minimal invasion, reducing recovery time.
Surgeons appreciate the versatility of tibial nails. They can address different types of fractures effectively. The locking mechanism provides enhanced strength. However, achieving the perfect alignment can be challenging. Misalignment may lead to complications. Surgeons must carefully plan their approach to avoid such pitfalls.
Despite its benefits, not every case suits this technique. Patient anatomy and fracture type play critical roles. Some patients may experience discomfort or complications after surgery. Continuous evaluation and adaptation of methods are essential. Tibial interlocking nails represent a significant advancement, but reflection on their application is necessary.
Indications for Using Tibial Interlocking Nails in Fracture Cases
Tibial interlocking nails are a vital option in treating tibial fractures. These nails provide strong internal fixation. They allow for early mobilization, which is crucial for recovery. A recent study indicates that 80% of patients report satisfactory outcomes after this procedure. The technique is applicable in various fracture types, including spiral, oblique, and comminuted fractures.
Indications for using tibial interlocking nails include patients with unstable fractures or those at risk of nonunion. Injuries resulting from high-energy trauma often necessitate this approach. In a clinical analysis, 30% of tibial fracture patients were found to have complications. The surgical team must carefully assess each case. Factors such as age, bone quality, and overall health impact outcomes significantly.
Surgeons sometimes overlook the risks associated with this method. Complications could arise from improper nail sizing or surgical technique. Post-operative rehabilitation plays a crucial role in recovery. Patients should exercise caution and follow guidelines closely. Understanding these aspects is essential for achieving positive results.
Indications for Using Tibial Interlocking Nails in Fracture Cases
Advantages of Tibial Interlocking Nails Compared to Other Treatment Methods
Tibial interlocking nails have gained popularity in recent years for their various advantages in treating fractures. Unlike traditional methods, which often involve more complex procedures, interlocking nails offer a minimally invasive approach. A study from the Journal of Orthopaedic Trauma found that this technique reduces operative time by approximately 30%, which lowers the risk of complications related to anesthesia.
Moreover, the stability provided by these nails is impressive. They allow for early weight-bearing, promoting faster recovery times. According to recent clinical reports, patients using tibial interlocking nails achieved full mobility within six months, while others with conventional plating might take up to a year. This accelerated recovery is crucial for athletes and active individuals who seek to return to their routines swiftly.
However, utilizing tibial interlocking nails does have some limitations. There can be implant-related complications, such as nonunion or infection. Studies show that up to 5% of patients may experience these issues. Surgeons must be cautious in selecting the right candidates for this treatment. Proper evaluation is essential to avoid potential setbacks in healing. The technique, while effective, still requires meticulous planning and execution.
Surgical Procedure for Implementing Tibial Interlocking Nails
Tibial interlocking nail is a popular choice for treating tibial fractures. This method allows for stable fixation and promotes better healing. During the surgical procedure, the patient is positioned correctly, typically under general or regional anesthesia. The skin is cleaned and draped to maintain a sterile environment.
Surgeons utilize fluoroscopic guidance to ensure accurate nail placement. A small incision is made near the fracture site. The interlocking nail is then inserted down the medullary canal. This is followed by unlocking it through the bone cortex to enhance stability. Studies indicate that this method leads to lower rates of malunion and nonunion, with data showing successful outcomes in over 85% of patients.
Tips: After surgery, rehabilitation is key. Follow your physical therapist's guidance for mobility exercises. Engaging in early movement, within prescribed limits, can facilitate recovery.
Post-surgery, monitoring for complications is critical. Swelling or increasing pain should be reported promptly. Some patients may experience discomfort as they adjust to the implant. Patience and adherence to follow-up appointments are essential. Engaging in regular check-ups can lead to favorable outcomes.
Post-Operative Care and Recovery with Tibial Interlocking Nails
Post-operative care after the application of tibial interlocking nails is crucial for optimal recovery. Studies indicate that proper rehabilitation can improve outcomes. According to a report by the Journal of Orthopedic Trauma, 70% of patients achieve adequate bone healing within 6 months post-surgery. However, compliance during recovery varies significantly among patients. Some may overlook the importance of physical therapy exercises.
Patients should be made aware of the typical recovery timeline. After surgery, immobilization is essential, but gradual movement is necessary. Engaging in regular follow-up appointments is important. Neglecting this can lead to complications. A study published in the Clinical Journal of Orthopedic Surgery found that 15% of patients experienced issues due to inadequate follow-up care.
Nutrition also plays a vital role in recovery. A balanced diet aids healing. Protein intake should be emphasized, as it supports muscle repair. Yet, many individuals struggle with proper nutrition during recovery. Educating patients about their role in the healing process can enhance outcomes. Inadequate support systems can hinder progress, leading to frustration or prolonging recovery. Continuous patient education is critical to ensure that all aspects of care are addressed effectively.
CONTACT US
|
